She was given combination pills and pelvic US which revealed 10 cm complex R adnexal mass.
No abdominal pain/fullness, weight loss or anorexia.
Menarche at age 13 with no hx of abnormal Pap or chlamydia/trich.
Obesity was noted.
Disorganized endocervical stroma with breakdown per endometrial bx.
Elevated LDH - 192.

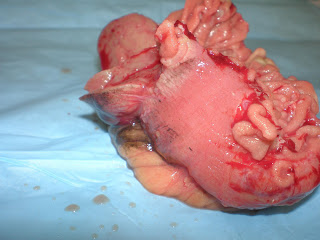
R oophorectomy specimen. Serous fluid when opened.
So when encountering teratoma,
1) if mature, then no further treatment needed.
2) if immature component seen in histology, treatment more aggressive. More lymph node dissection and adjuvant therapy.
In immature teratoma, malignancy mostly arise from neural component.

This specimen shows multiple dermoid cysts each spitting out sebum with hair when opened.


There was also a tooth(that dark spot) where I palpated. Either tooth or just calcification.
Frozen section showed sebaceous glands, smooth muscle, ovarian stroma, pancreas, colon, brain, hobnailing area that looked choroid plexus(?) and small lymphoid cells but had clear vacuole in the nucleus. Pleomorphic and less differentiated, diagnosis was mature teratoma with focal area suggestive of immature element.
Ovarian stroma


Sebaceous glands with hair shaft and smooth muscle around.

fibroadenomatous.

tubal

intestinal

pancreatic acini

neural
so far these looked well differentiated until we reached a focus around neural tissue.