LFT enzymes
Liver Necrosis
Liver Disease Characteristics
Vascular Liver Dz
Acute vs Chronic Hepatitis
Bacterial Infection Route
Patterns of Chronic Hepatitis
Metabolic Liver Disease - hemochromatosis, Wilson's dz
Cirrhosis
Biliary Cirrhosis
=======================================
main rate limiting step in bilirubin metabolism is excretion by the canaliculi rather than conjugation
- alkaline phosphatase - located on the cell membrane of biliary canaliculi
- transaminase - located in the hepatocyte cytoplasm, ALT more specific for liver than AST
- conjugated bilirubin - secreted by liver cells associated with biliary obstruction or liver cell destruction
- albumen - reflects synthetic property of liver, low level => long standing disease of liver
- caeruloplasmin
- transferrin
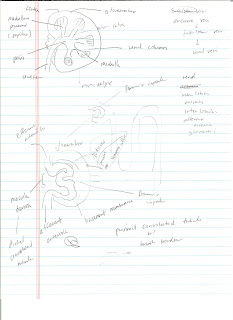
space of Disse
between hepatocyte surface and endothelial lining of sinusoid (larger than capillaries)
Liver Necrosis
- councilman bodies - dead hepatocytes form eosinophilic shrunken structure
- spotty necrosis - patchy
- zonal necrosis - necrosis confined to zone
- piecemeal necrosis - scattered pattern immediately next to the portal-tract connective tissue
- bridging necrosis - extensive necrosis that bridge different veins/tracts
General Liver Disease Characteristics
- fatty change
- cholestasis
- extrahepatic
- intrahepatic
- liver necrosis
- liver fibrosis - cells of Ito in space of Disse
- liver storage disease
- hemochromatosis, hemosiderosis, Wilson's disease
- glycogenesis (glycogen storage dz)
Vascular liver disease
- true infarct - rare, from trauma, arterial embolization, bacterial endocarditis, eclampsia, polyarteritis nodosa(Kussmaul disease)
- R sided heart failure -> passive venous congestion of liver -> nutmeg appearance (chronic passive venous congestion)
- portal HTN
- increase in portal venous pressure
=> splenomegaly, ascites
- new channels may open up betweeen portal and systemic venous circulation
- variceal bleeding
- caput medusa
- hemorrhoids
- classified: pre-sinusoidal, sinusoidal or post-sinusoidal
EXAMPLES: PRE-SINUSOIDAL - PORTAL VEIN THROMBOSIS
SINUSOIDAL - HEPATIC FIBROSIS, CIRRHOSIS
POST SINUSOIDAL - HEPATIC VEIN THROMBISIS, CENTRAL VEIN THROMBOSIS
Clinical Picture: Budd-Chiari Syndrome (post sinusoidal)
TRIAD: 1) ABD PAIN
2) ASCITES
3) HEPATOMEGALY
--------------------------------------------------------
ACUTE HEPATITIS
- INCREASED BILIRUBIN
- INCREASED ALT/AST - LIVER CELL NECROSIS
- ALBUMEN ~ NORMAL
- DECREASED COAGULATION DUE TO DECREASE IN COAGULATION FACTOR PRODUCTION
Hepatrophic Virus
A, E = fecal, oral
B, C, D = parenteral, histologically ground glass apperance of hepatocytes (accumulation of antibodies)
Route of Bacterial Infection
- ascending from biliary tract
- ascending in the portal vessels from a focus of sepsis in abdomen
- systemic septicemia
3 histological Patterns of Chronic Hepatitis
- chronic active hepatitis
- continued necrosis of hepatocytes
- development of cirrhosis
- necrosis extends from one portal area to another, portal tract to parenchyma
- chronic persistent hepatitis
- confined to portal tract
- not associated with progressive fibrosis or cirrhosis
- chronic lobular hepatitis
- portal tract inflammation(no piecemeal necrosis), spotty parenchymal inflammation
Metabolic Liver disease
Iron - hemochromatosis
primary - excessive absorption of iron(accumulates as hemosiderin) from gut
- chromosome 6, HLA locus
- cells look rusty brown due to hemosiderin in cells
- great increase transferrin in blood, increase of iron, ferritin
secondary - also called hemosiderosis
- due to other disease (alcoholism) or repeated blood transfusion
Copper - Wilson's disease
- decrease in ceruloplasmin (Cu binding) in blood
- liver fails to excrete
- Cu-ceruloplasmin complex
- overspills into blood, deposited in brain, cornea
Cirrhosis hx
- long destruction of liver cell
- chronic inflammation stimulating fibrosis
- regeneration of hepatocytes to form nodules
Biliary Cirrhosis
- Secondary - obstructed extrahepatic duct
- Primary - Autoimmune, Slow destruction of bile canaliculi
- sclerosing cholangitis
- associated with inflammatory bowel disease
- both intra/extra hepatic duct
- medium sized ducts, ducts in portal tract => concentric fibrosis and inflammation, small ducts => replaced by collagen, fibrous stricture with segmental dilatation